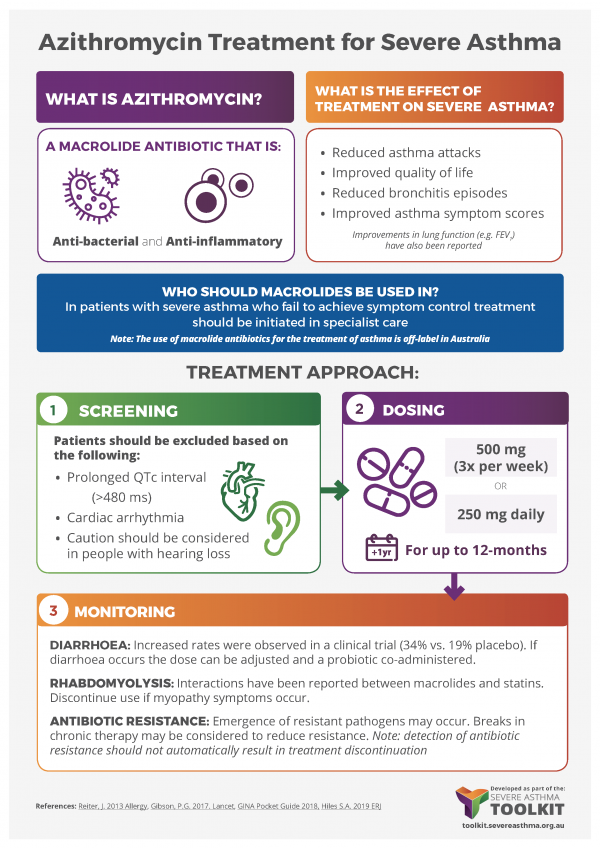
Clinical Recommendations for The Use of Azithromycin in Severe Asthma in Adults
NOTE: The use of macrolide antibiotics, including azithromycin, for the treatment of asthma is off-label
Download the pdf document here: Macrolide Recommendation Version 1 (24 October 2019)
Note: An overview video on macrolide treatment for asthma is available on the Centre of Excellence website: https://www.severeasthma.org.au/macrolides-severe-asthma/